Symptomatic Gallstones
Biliary colic - is the pain experienced when contraction of the gall bladder causes stones to temporarily obstruct the outlet of the gall bladder blocking the passage of bile. This pain typically comes and goes in waves without ever fully dissipating. It begins in the epigastrium (upper middle abdomen) and can remain localized but may also radiate under the right costal margin. It is usually triggered by a meal and particularly fatty meals, it may be associated with nausea and diarrhea but this is not common.
Cholecystitis - if a gallstone becomes stuck in the outlet of the gallbladder it causes a constant blockage and an inflamed gallbladder ensues. This pain is constant and localized to the right upper quadrant of the abdomen, if this constant pain is ongoing for 48hours diagnostic certainty is greatly increased.
Pancreatitis - tiny gallstones pass along the common bile duct, just before they reach the opening into the duodenum they pass through a common channel with the pancreatic duct and thus can lead to irritation and inflammation of the pancreas. Classically, this pain is sudden onset and severe, it starts in the epigastrium & radiates to the back and is strongly associated with nausea and vomiting.
Risk factors of gallstone disease

It is estimated that up to 20% of the adult population have gallstones, however only 20% of this group are symptomatic and thus require cholecystectomy. The adults who are at increased risk of developing gallstones fall into these categories-
- Over 40years old (4-10 times more likely)
- Female (2 times more likely)
- Family history (5 times more likely)
- Obesity and rapid weight loss
- Type 2 diabetes
- Liver cirrhosis
- Crohn’s disease
- Cystic fibrosis
- Drugs- thiazide diuretics, ceftriaxone & oral contraceptive pill
How gallstones form

Gallstones form due to supersaturation of bile with either cholesterol or bilirubin.
Cholesterol stones are most common (70% of stones), conditions that lead to increased secretion of cholesterol (such as obesity and type 2 diabetes). Bile salts are what allows cholesterol to remain soluble in the bile and a decline in these salts (conditions such as Crohn’s disease and Cystic fibrosis that prevent bile salt absorption from the intestine) can also lead to stone formation.
Pigmented stones are formed by conditions that lead to increased secretion of bilirubin and are not as common as cholesterol stones. This occurs due to increased breakdown of haemoglobin found in red blood cells as seen in diseases such as sickle cell anemia where prophylactic cholecystectomy should be considered. Mixed stones can also form primarily in the common bile duct and are due to recurrent ductal infections however this is seen more frequently in East Asia.

Finally, increased absorption of water from the gallbladder can lead to crystal formation such as in states of prolonged dehydration, bile stasis due to lack of contraction of the gallbladder prolonged fasting also contributes.
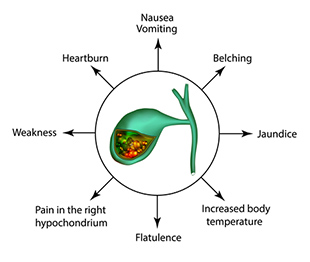
Complications of gallstone disease

- Biliary colic
- Cholecystitis
- Choledocholithiasis (stones in the common bile duct)
- Ascending cholangitis (infection associated with stones in the duct)
- Pancreatitis
- Mirizzi syndrome
- Gallstone ileus
- Porcelain gallbladder
Diagnosis of gallstone disease

Typically all that is needed to diagnose gallstone disease is
- Blood test - specifically liver function tests (LFT’s) &
- Ultrasound
Other tests that may be needed for difficult to diagnose symptoms
- MRCP - Magnetic Resonance Cholangiopancreatography
- CT IVC - Computed Tomography with intravenous cholangiogram
- HIDA scan - Hepatic Iminodiacetic Acid Scan (for functional gall bladder disorders)
Laparoscopic cholecystectomy with intra-operative cholangiogram

Surgery for gallstone disease is only indicated if the patient is symptomatic.
The operation is performed under a general anaesthetic with four keyhole cuts being made in the upper abdomen. The gall bladder is retracted up and away from the duodenum and important anatomical landmarks identified. A dissection is carried out defining the cystic duct and cystic artery and then a cholangiogram study is performed, this involves taking a series of x-rays as dye is injected into the biliary system via the cystic duct. After the cholangiogram is finished, clips are placed on the cystic duct and artery before they are divided. The gall bladder is dissected off the liver, placed in a bag and then extracted from the abdomen. The operative area has a final inspection before the abdominal wounds are closed with dissolvable sutures and dressings applied.
Post-operative diet and recovery
All patients are commenced on a normal diet after surgery. Most patients can be medically cleared to go home the same day however it is entirely reasonable if a patient wishes to stay overnight in hospital. For people who work in an office, one week off is usually all that is required and patients can commence driving 4-5 days after surgery once they are confident any pain from their incision sites will not distract them from the road. Walking is encouraged from day one however waiting at least one month before activating your core muscles with resistance training is advised in order to reduce the risk of hernia.
Same day gallstone surgery

As we have on-site pathology and medical imaging at Lakeview Private hospital, pre-operative investigations and surgical review can be arranged immediately on the patient presenting to Circle of Care.
Circle of Care is able to provide streamlined access to surgery as we operate Mondays, Wednesdays and Fridays at the hospital. This means patients can save money from not having to pay emergency department fee’s that are non-refundable. It also saves patients spending an unnecessary night in the hospital ward before getting the surgery they need.


